Community Pharmacy Cooperative’s Chief Pharmacy Officer Tom Siepka shares his opinion in this Boston Globe story on the efficacy of pharmacy benefit managers and their programs, and if they are a benefit to community health center patients throughout the United States.
The pharmaceutical industry is pushing back on a program that allows community pharmacies, like one in Brockton, to purchase drugs at steep price cuts
BROCKTON — Since the Brockton Neighborhood Health Center opened its own pharmacy more than a year ago, the facility has acted as an oasis for a community that sorely lacks drugstores.
As CVS, Walgreens, and Rite Aid closed hundreds of stores across the state in recent years, nonprofit community pharmacies like the one in Brockton — and others in Dorchester, South Boston, and Roxbury — have stepped up to fill the void.
RelatedWhen drugstores disappear: Why nearly 15,000 Bostonians live in ‘pharmacy deserts.’
But they face an uncertain future. Drug companies and front-line providers have been battling over a rapidly growing federal program that these centers rely on — and that costs the pharmaceutical industry tens of billions of dollars each year.
The program, known as 340B, allows community pharmacies to purchase drugs at steep price cuts. But pharmaceutical firms have been heavily lobbying Congress to limit how community pharmacies distribute high-cost drug treatments to patients beyond their physical walls. In a recent congressional hearing, some lawmakers said they might support restricting the program, which could squeeze the finances of places like the Brockton center.
Meanwhile, in the Massachusetts State House, a lawmaker recently introduced an amendment supported by the drug industry that severely restricts how 340B pharmacies can use such discounts. Observers say there is a good chance that at least some of these efforts could pass this year.
Efforts to cut back that program could not only deprive patients of affordable life-saving medications but also cut off an important revenue stream for community pharmacies, said Tom Siepka, chief pharmacy officer of the Community Care Cooperative, a Boston-based organization that supports health centers.
“Without it, I don’t know how these pharmacies stay open,” Siepka said. “The program is a critical lifeline.”
Founded in 1992, the drug-discount program requires drug makers to offer discounts as high as 25 to 50 percent to hospitals and pharmacies that serve a relatively high number of low-income patients.
The Brockton center acquires about 75 percent of its prescriptions through these federally mandated discounts, with the savings reinvested in lower drug prices for patients, new technology, interpreters, and free home delivery.
“Patients are able to get their medication more quickly, more efficiently, in a language they understand with a team that they trust,” said chief medical officer Joseph Panerio-Langer.
Danielle McGrath counts herself as pretty lucky. The 32-year-old only has to walk 10 minutes once a week to pick up her medications and talk to a pharmacist at the Brockton center.
“The people there are so helpful to me,” McGrath said. “It’s a lot easier to get my prescriptions now.”
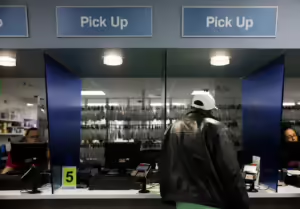
Pictured above: Patient picked up a prescription at Brockton Neighborhood Health Center’s
pharmacy. As pharmacies, both corporate and independent, close in underserved communities
of color, Brockton Neighborhood Health Center stands out as a rare success story.
Jessica Rinaldi/Globe Staff
Today, the pharmacy serves about 39,000 patients and dispenses about 1,000 prescriptions a day, more than three times the average volume at a CVS or Walgreens. The facility even employs a high-tech robot that organizes deliveries.
But the rapid expansion of the discount program has drawn the ire of the drug industry, which fully pays for 340B. In 2022, health care organizations purchased $53.7 billion worth of discounted outpatient drugs, compared with $9 billion in 2014, government data show. 340B now represents the largest federal prescription drug program.
One reason for the explosive growth: the rapid emergence of “specialty drugs,” a term developed by the industry to describe innovative, high-cost treatments for chronic, complex diseases such as cancer, rheumatoid arthritis, HIV, and hepatitis C.
Over the past decade or so, specialty drugs have become a boon for major pharmaceutical firms including Merck, Johnson & Johnson, Pfizer, and Eli Lilly. Today, such drugs account for more than 50 percent of all drug spending, a figure that exceeds $300 billion.
Many hospitals and community pharmacies such as the one in Brockton that receive the federally mandated discounts can’t sell specialty drugs because they lack the necessary expertise to administer such sensitive treatments, which can carry potentially significant side effects. Instead, they contract out these prescriptions to for-profit Walgreens, CVS, Walmart, and Rite Aid stores and split the fees.
These sorts of arrangements — combined with a change under the Affordable Care Act that allowed providers to contract with unlimited pharmacies to obtain the cheaper drug prices — have contributed to a rapid expansion of pharmacies receiving the discounts: 30,000 in 2021 compared with under 1,300 in 2010, according to an analysis by Drug Channels Institute.
Alarmed at the growing costs, the pharmaceutical industry has been pushing back, saying the federal discount program has strayed from its original purpose.
“Since 2010, we’ve seen the program shift to being a profit stream for hospitals and the pharmacies they interact with,” said Nicole Longo, a spokesperson for Pharmaceutical Research and Manufacturers of America. “We want the discounts to go to patients that need them, which are the low-income and uninsured.”
Drug giant Pfizer is funding efforts by the Pioneer Institute in Boston to track 340B discounts. The free-market think tank compiled data that it says show 61 percent of such pharmacies in Massachusetts are located in affluent neighborhoods, including Wellesley and Swampscott. Patients there often have private insurance, which pays higher rates for drugs that the pharmacies acquire at the same discounted price as they would for Medicaid patients.
Drug makers have been pushing officials to limit the number of pharmacies a hospital or health center can contract with to just one, according to the Congressional Research Service.
Congress is also considering several bills aimed at reforming the program. A bipartisan group of senators has crafted a bill that would codify drug makers’ obligations to sell drugs at discounted prices but also require regular audits.

Pictured Above: Pharmacist Damian Mitrano refilled Parata, the
Brockton Neighborhood Health Center pharmacy’s robotic drug dispensing system.
Jessica Rinaldi/Globe Staff
In June, a Republican-led House subcommittee signaled support for a bill favored by the pharmaceutical industry that would require hospitals to report how they use their savings from discounts. It would also clarify eligibility requirements in a way that could restrict the discounts.
Siepka of Boston’s Community Care Cooperative said any effort to restrict the number of pharmacies that providers can contract with will ultimately hurt the finances of places such as the Brockton clinic.
Pharmacies often lose money on drugs because the payments they receive from insurance companies don’t cover the full cost of purchasing and administering the prescriptions. Therefore, contracting out discounted specialty drugs offers them a crucial source of revenue.
“For many of these pharmacies, their finances hang on a string,” Siepka said.
Experts say nonprofit community pharmacies need to survive, especially as CVS, Walgreens, and Rite Aid continue to close stores. They could never replace large chains — CVS alone operates about 400 drugstores in Massachusetts, while there are roughly 50 community health centers — but these mission-driven facilities can alleviate the harms when for-profit pharmacies close.
“We feel the solution to pharmacy (closures) is to invest in health centers and expand their pharmacies,” said Michael Curry, chief executive of Massachusetts League of Health Centers.
The financial stability of these centers, then, is critical for patients.
Ellen Lapre, 61, who requires treatment for conditions related to her blood pressure, cholesterol, and thyroid, recently decided to switch from a CVS in Bridgewater to the Brockton center.
“The staff (at Brockton) is amazing,” Lapre said. “They didn’t seem to care about the bottom line or what insurance you had. They just wanted to make sure you got your meds.”
By Globe Staff, Updated July 30, 2024, 7:31 a.m.